A Pain in the Nut(s)
/A quick note from Sarah: We’re pleased to present a blog post from a non-pelvic PT! We’ve had great chats with Steve at PT Pub Nights in the past, and were thrilled when he asked about sharing his experience. Of course, I’m personally always happy to see more support for my feelings that ALL physical therapists are pelvic health therapists is some small way. I’d also like to apologize to Steve, who wrote this blog quite sometime ago, and I have been slow to publish. Thank you for your post, and your patience!
A Pain in the Nut(s)
Steve Goostree, DPT, OCS, Cert. MDT, FAAOMPT
stevegoostree@gmail.com
I was inspired to write up and share a case I recently encountered after a conversation at PT Pub Night, sponsored by the lovely Sarah Haag and Sandy Hilton of Entropy Physiotherapy.
The patient was a healthy 24 y/o male that reported to PT with primary complaints of right testicular pain. He was referred by his PCP after a routine physical examination, which deemed his testicular pain as non-sinister. No imaging had been obtained, and the patient was not taking any medication. Past medical history was insignificant. He noted a recent gradual onset of right testicular pain after starting a new weightlifting regimen in the gym within the past month. The patient scored low on the Yellow Flag Questionnaire, indicating low psychosocial factors contributing to his pain. Special questions including bowel and bladder habits, swelling or change in structure were all negative. The patient did report a sedentary desk job, where he felt some lower back stiffness, which resulted in an increase in his testicular symptoms as th day progressed.
Being trained as an orthopedic manual PT, I was slightly uncomfortable performing a male pelvic exam, and was taught to always rule out the spine first as a primary source of referred pain. Before making this an uncomfortable experience for the patient and myself alike, I trusted my gut and screened the lumbar spine first. Having the patient actively cough was used as a symptom provoking baseline.
Lumbar AROM with overpressure was normal, except a positive right lumbar extension quadrant with overpressure, resulting in familiar right testicular complaints, rated 5/10 via NPRS. Sensation, myotome and DTR testing were all normal. Right unilateral passive accessory mobility pressures near L2-3 produced familiar symptoms radiating to the patient’s right testicle.
A repeated movement examination of the lumbar spine was performed next. After 30 repeated extensions in lying with clinician overpressure, the patient was asked to sit up and cough. He noted a decrease in symptoms. A right lumbar quadrant test with overpressure was reassessed, and the patient now noted a pain level of 2/10 via NPRS.
The patient was issued repeated extension in lying, using a belt for self overpressure 10 reps 5-6x/daily. The patient was seen for 3 visits, which included oscillatory mobilization targeting the right upper lumbar segments (Gr. III per Maitland) and a HEP following the lumbar extension principle with progression of forces as needed. Proper lifting technique in the gym was also reviewed as recovery of function. The patient stated he was ready for discharge after visit 3.
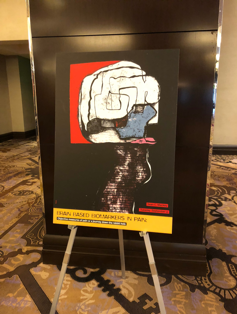
This brief case highlights the importance of a thorough spine screen for the orthopedic and pelvic health therapist, which is quick, easy and should be a day one priority for any neuromusculoskeletal complaint. The exact mechanism as to why this intervention was effective is unknown, but reviewing the photo may explain things anatomically. As always, further research is needed.